Home Health Care Nursing: Your Guide to In-Home Medical Support
Outline and How to Use This Guide
Home health care nursing brings hospital-grade skills to familiar rooms and routines. The aim is practical: stabilize health, prevent complications, and help people live well where they are most comfortable. To make this resource useful whether you are a family caregiver, a patient considering options, or a community professional, the guide begins with an overview and then moves through key decisions. Think of it as a map you can fold into your pocket—clear landmarks first, then details you can reference when questions arise.
This article is organized to balance clarity with depth. It starts by defining what home health care nursing includes and how it differs from non-medical home support. Next, it examines benefits, limitations, and real-world outcomes, taking care not to overpromise. Then it opens the door to a typical visit so you can picture what happens and why. Finally, it walks through how to arrange services, what to ask providers, what coverage may look like, and how to coordinate care without losing sleep.
Here is the roadmap at a glance:
– Section 2: A plain-language definition of home health care nursing, how licensure and scope of practice work, and how it compares to clinic, hospital, and non-medical home care.
– Section 3: When in-home nursing is appropriate, what evidence shows about safety and outcomes, and how to weigh home-based support against facility-based recovery.
– Section 4: What to expect during a visit, from assessment to wound care, medication reconciliation, and education, including tools, documentation, and infection control.
– Section 5: Steps to start, referral pathways, common coverage scenarios through public and private insurers, care plan coordination, and a concise conclusion for next moves.
Use the sections in sequence if you are just starting out, or jump to the parts that match your current decisions. Throughout, you will find short lists that distill complex choices into manageable actions. The goal is to help you ask informed questions, set realistic goals, and partner effectively with a nurse who meets you at your doorstep, not in a waiting room.
What Home Health Care Nursing Is—and What It Isn’t
Home health care nursing is skilled, short- or medium-term medical support delivered where a person lives. It is provided by licensed nurses who can perform clinical assessments, manage medications, dress wounds, educate patients and caregivers, and coordinate with physicians and therapists. Crucially, care is guided by a written plan developed with the ordering clinician and adjusted as health changes. The nurse’s visit is not a social call; it is a structured clinical encounter adapted to a home environment.
Because terms can blur, it helps to draw clear lines. Non-medical home care focuses on daily activities—bathing, meals, rides, light housekeeping. In contrast, home health care nursing addresses medical needs—symptom monitoring, injections, ostomy support, catheter care, or intravenous therapies when appropriate. Clinics offer scheduled evaluations; hospitals deliver intensive, continuous monitoring; home health care nursing sits between, offering episodic skilled care plus education designed to help people and families manage safely between medical appointments.
Credentials and scope matter. Registered nurses conduct comprehensive assessments, oversee complex interventions, and triage emerging issues. Licensed practical or vocational nurses may carry out specific treatments under supervision according to local regulations. All operate within state or national practice acts and follow physician or advanced practitioner orders. This framework protects patients while allowing flexibility; a living room can become an efficient, lower-stress care setting when the right skills and safeguards are in place.
Consider common scenarios: a person returning from surgery who needs incision checks and pain management titration; an older adult with heart failure learning to balance fluid intake, daily weights, and medications; a person with diabetes working on glucose patterns, foot care, and meal planning; or a patient with a chronic wound requiring staged dressings and infection surveillance. In each case, the nurse’s role is to translate clinical goals into doable steps at home. It is not round-the-clock supervision, and it is not a substitute for urgent or emergency care. Instead, it is targeted, time-bound, and coordinated—medical help that meets life where it happens.
Benefits, Limits, and When Home-Based Nursing Fits
When it is appropriate, home health care nursing offers a mix of comfort and clinical focus that can be hard to replicate elsewhere. Familiar surroundings reduce disorientation, especially after hospital stays. Family members can learn beside the nurse, building confidence in daily routines like medication timing or wound care steps. Travel time drops, which is meaningful for people with mobility challenges or limited transportation options. For many, the most compelling advantage is continuity: the same nurse or small team seeing you where you live, noticing patterns that might be invisible in a 15‑minute clinic slot.
Evidence aligns with these experiences. Health services research has reported that structured home health programs for selected conditions are associated with lower rates of short-term hospital returns, often in the single to mid‑teens percentage range relative to usual care, depending on diagnosis, severity, and program design. Preventing even one avoidable readmission conserves energy, reduces risk, and can lower overall costs. Education delivered at home tends to stick because it is tailored to your kitchen, your pillbox, your schedule—context that transforms instructions into habits.
That said, home care nursing is not a cure-all. It works best when needs are skilled but stable between visits. People requiring continuous monitoring, advanced imaging, or complex procedures may be safer in inpatient settings. Some homes present barriers—stairs without rails, poor lighting, limited refrigeration for medications—that need mitigation before services can begin. Geographic access varies; rural areas may see longer wait times. And while many public and private insurers cover clinically necessary home health episodes, coverage rules, visit frequencies, and duration limits differ, so benefits should be confirmed up front.
A practical way to judge fit is to match goals with support level. If the aim is to recover from an acute event, learn self-management for a chronic condition, or receive intermittent treatments with oversight, in-home nursing can be among the top options. If the goal requires rapid diagnostics, continuous observation, or immediate escalation, a clinic or hospital may be the safer route. The value lies in right-sizing care: enough skill to prevent setbacks, delivered where daily life actually unfolds.
Inside the Visit: What Skilled Nursing Looks Like at Home
A home health nursing visit is structured, even if it begins with a warm greeting and a quick check on how the morning went. The nurse typically starts with vital signs and symptom review, scanning for trends rather than isolated numbers. A head‑to‑toe assessment follows as needed, tuned to the reason for care: lungs for breathlessness, legs for swelling, skin for pressure risk, cognition for changes that could signal infection or medication effects. The setting is informal, but the clinical lens is focused.
Treatments and teaching are the core of the encounter. Wound care is common and precise—measuring, cleansing, selecting dressings that balance moisture and protection, and documenting progress with consistent methods. Medication reconciliation threads through the visit: verifying doses, sorting duplicate prescriptions, matching labels to the latest care plan, and using simple tools like pill organizers to reduce confusion. For chronic conditions, education is woven into each step: why daily weights matter in heart failure, how to time meals and insulin for diabetes, what red‑flag symptoms mean and when to call.
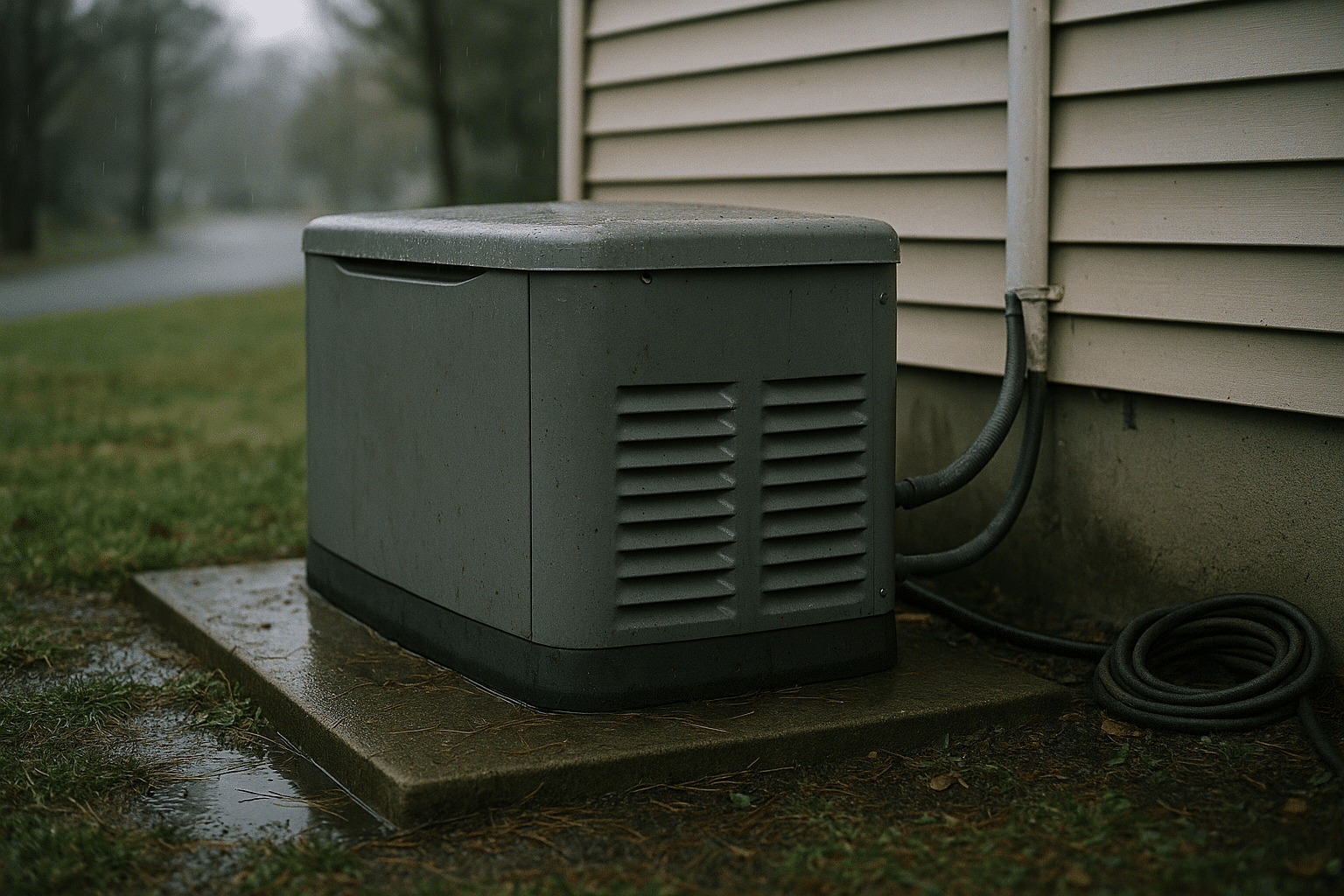
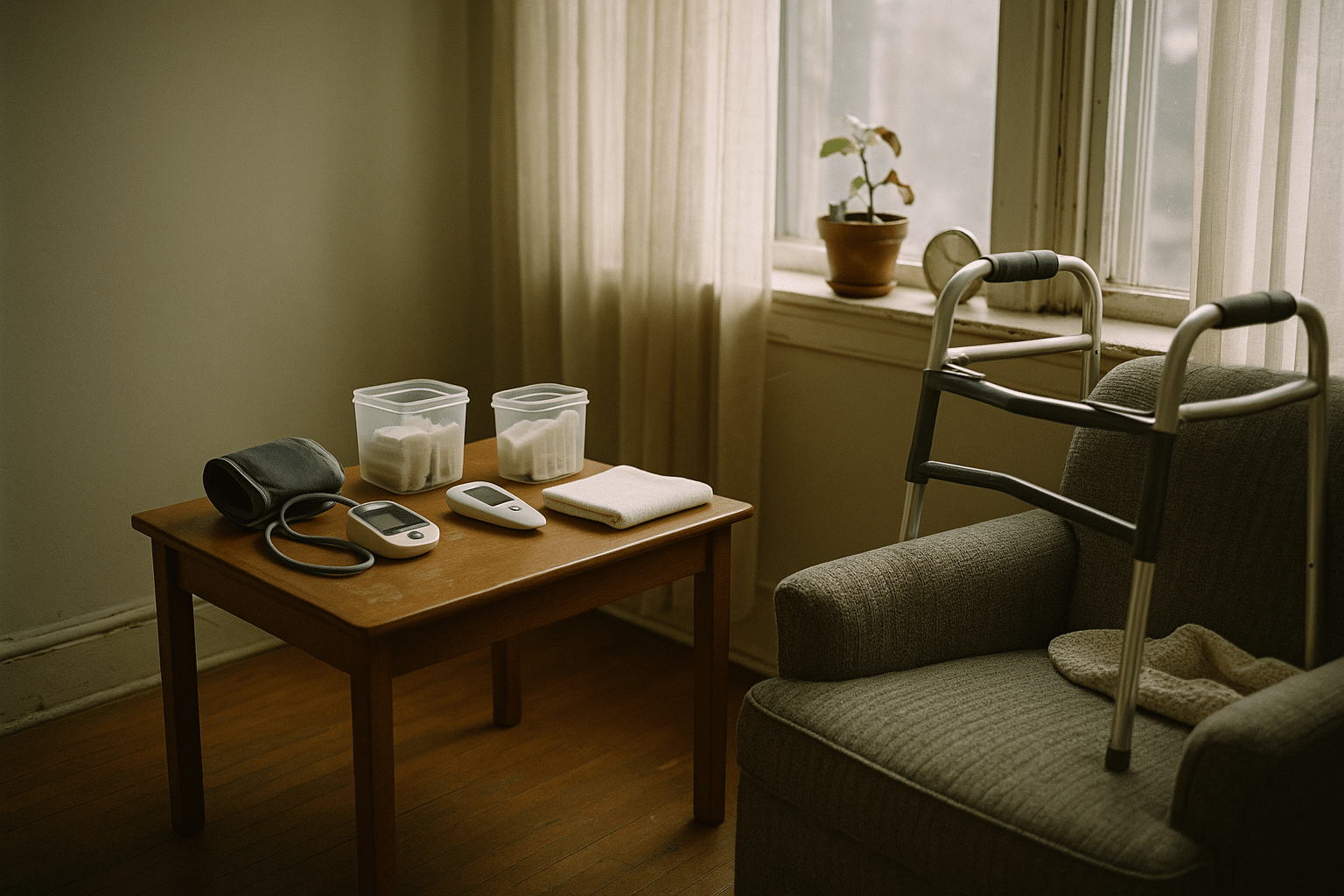
Expect practical tools, not a rolling hospital cart. Portable blood pressure cuffs, pulse oximeters, sterile dressing kits, and compact scales are common. Some programs add remote monitoring so daily metrics reach the care team between visits; others rely on call check‑ins and symptom logs. Infection control is a constant: hand hygiene, clean work surfaces, and safe disposal of sharps. If home equipment is involved—oxygen concentrators, walkers, bathroom grab bars—the nurse will check setup and safety.
Documentation may feel quiet but is crucial. The nurse records findings, treatments, patient response, and education provided, then updates the plan with the ordering clinician as needed. Coordination often extends beyond the doorway: a message to the prescriber about blood pressure trends, a referral to physical therapy, or a timely order for lab work. You will also leave each visit with clear next steps, often summarized in plain language. To keep it tangible, many nurses use simple checklists you can post on the fridge:
– Today’s actions: what was done and why.
– Daily routine: meds, measurements, movement, meals.
– Warning signs: when to call the agency or go to urgent care.
– Follow-ups: upcoming visits, tests, or adjustments to expect.
In short, the visit is an hour where clinical precision meets everyday life—a small, repeatable rhythm that helps keep bigger disruptions at bay.
Getting Started, Paying for Care, and Coordinating the Team
Arranging home health care nursing begins with a clinical order. This may come from a hospital discharge, a primary care office, or a specialist who believes skilled support at home can speed recovery or stabilize a condition. A coordinator conducts an intake, confirms basic eligibility, and schedules the first visit. Before that visit, set the stage: clear a small workspace at a table, gather the current medication list and recent paperwork, and note top concerns so nothing important gets lost in the moment.
Coverage varies by insurer, but many public and private plans pay for time‑limited, medically necessary home health episodes ordered by a clinician. Typical requirements include a documented need for skilled services, a condition that can be safely managed between intermittent visits, and a plan of care with measurable goals. Out‑of‑pocket costs depend on the policy and any deductibles or copays. If you are uninsured, ask about community programs or sliding‑scale options; some local agencies partner with charities or public health funds to bridge gaps.
To choose wisely, compare agencies on transparent criteria rather than glossy brochures. Useful questions include:
– What services are provided by licensed nurses, and how are visit frequencies determined?
– How do you coordinate with physicians, therapists, and pharmacists?
– How do you handle after‑hours concerns and urgent changes?
– What outcomes do you track for conditions like wounds or heart failure, and how do you share results?
– How do you support caregiver training and respite?
Once services begin, communication is the glue. Keep a shared notebook or digital log so everyone sees the same medication lists, symptoms, and goals. Align targets that matter: fewer breathless nights, a wound that shrinks week to week, energy to walk to the mailbox without stopping. Revisit the plan every couple of weeks; home health is designed to step down as skills and stability improve. If needs increase, the nurse can recommend clinic follow‑up, additional therapies, or safer alternatives.
Conclusion: Making Home the Center of Care
For individuals and families weighing options, home health care nursing can be a well‑regarded way to blend medical oversight with daily life. It delivers structured skill without uprooting routines, teaches in the context that matters, and coordinates a team around your goals. Start with a clear order, verify coverage, ask pointed questions, and keep communication open. With the right match, your home becomes a place where healing is not only possible, but practical.