Senior Care: A Guide to Understanding Support Options for Older Adults
Outline
– Why senior care choices matter and how to start
– Assessing needs and risks
– Staying at home with community and in‑home supports
– Community and residential living options
– Paying for care and managing trade‑offs
– Bringing it together with a practical roadmap
Introduction
As families live longer and communities evolve, decisions about senior care arrive sooner and feel more complex. The goal is simple—safety, dignity, and a life that still feels like one’s own—but the paths to get there vary. Some older adults thrive with modest tweaks at home; others benefit from structured support or a residential setting designed for round‑the‑clock needs. This guide translates the maze of services into plain language, helping you weigh independence, health, and cost. It offers checklists you can use today and examples that show how different supports fit real lives. If you’re switching between doctor visits, work calls, and late‑night “what now?” searches, consider this your calm companion and practical playbook.
Assessing Needs and Risks: Turning Observations into a Care Map
A thoughtful plan begins with observation. Rather than guessing, convert daily life into data you can act on. Start with activities of daily living (ADLs): bathing, dressing, toileting, transferring, continence, and eating. For each, note whether the person is independent, needs reminders, or requires hands‑on help. Then review instrumental activities of daily living (IADLs): managing medications, cooking, shopping, handling finances, housekeeping, and using transportation. These tasks often slip first and are strong early signals that support is needed.
Next, scan health and safety. Falls are a leading cause of injury for older adults, and even a “minor” stumble can spark a chain of setbacks. Check footwear, clutter, rug edges, loose cords, and lighting. Ask about dizziness, pain, and sleep. Vision and hearing changes can masquerade as forgetfulness, so consider whether new glasses, brighter bulbs, or hearing support would change the picture. Cognitive changes deserve gentle attention: missed appointments, getting turned around in familiar places, repeated questions, or unopened mail can point to memory or attention challenges.
To frame priorities, discuss what matters most. Some value staying in a beloved home above all; others prize easy access to social life or medical care. Write a one‑page summary: key diagnoses, medications, allergies, emergency contacts, and care preferences. Add realistic goals for the next 90 days, not forever. A compact plan clarifies decisions and makes conversations with clinicians more productive.
Use a quick checklist to guide your next step:
– ADLs: Where is help needed daily, occasionally, or not at all?
– Home safety: Are there tripping hazards, poor lighting, or tricky stairs?
– Health: Are pain, shortness of breath, or medication side effects limiting activities?
– Cognition: Are bills unpaid, meds missed, or routes forgotten?
– Social: Is there isolation, boredom, or lack of purpose?
When you map these factors, patterns emerge. Globally, the share of people aged 60+ continues to rise, and with longevity comes both opportunity and complexity. A structured assessment transforms worry into a navigable plan.
Staying at Home: In‑Home and Community Supports
For many, “home” is more than a place—it’s identity, routine, and memory. With targeted support, aging in place can work well. In‑home personal care aides assist with bathing, dressing, meals, light housekeeping, and companionship. In many regions, hourly rates fall in a mid‑range but vary by training and schedule; expect higher costs for nights, weekends, or specialized needs. Short, consistent visits can prevent crises by keeping nutrition, hygiene, and medications on track.
Skilled services at home—such as nursing visits, rehabilitation after a hospital stay, or wound care—are typically ordered for medical reasons and occur time‑limited. They differ from ongoing personal care, which focuses on daily living. Community services fill gaps: adult day programs offer social engagement, cognitive stimulation, and supervised activities while providing family caregivers a much‑needed break. Meal deliveries, transportation rides, friendly check‑in calls, and senior center classes can counter isolation and keep routines lively.
Home modifications stretch independence. Think small changes with big impact: grab bars in the bathroom, a second stair rail, non‑slip flooring, a handheld shower, and brighter task lighting. Larger projects might include a ramp, a zero‑threshold entry, or converting a first‑floor room into a bedroom. Costs range from modest to significant; a quick home safety walk‑through often uncovers low‑cost fixes worth doing immediately.
Technology can be helpful when chosen thoughtfully. Options include medication reminders, stove auto‑shutoff devices, motion‑sensing lights, and simple sensors that alert trusted contacts if a door opens at odd hours. Always weigh privacy, consent, and ease of use—if a gadget frustrates the user, it will gather dust. A home approach fits especially well when:
– Health is stable and predictable.
– Help is available for specific tasks at regular times.
– The layout can be made safe with reasonable changes.
– Social connection is maintained through routine outings or programs.
With the right mix, home can remain the heart of daily life while safety nets quietly hum in the background.
Community and Residential Living: Comparing Settings and Services
When needs outgrow what home can provide—or when loneliness or caregiver burnout sets in—community and residential settings offer structure along with social life. Independent living communities emphasize lifestyle: private apartments, meals available, activities, and maintenance‑free living. Assisted living adds daily help with bathing, dressing, and medications, plus staff on site at all hours. Memory‑support neighborhoods provide secure layouts, simplified cues, and programs designed for cognitive changes. Skilled nursing facilities deliver 24‑hour clinical oversight for complex medical needs, while short‑stay rehab units focus on recovery after illness or surgery. Some campuses offer multiple levels in one place, allowing moves as needs change.
Comparing settings is like comparing toolkits; the right match depends on what you need most. If managing pills and meals is the main challenge, assisted living’s structure can be a good fit. For wandering risk or disorientation, a secured memory program may reduce hazards and stress. If frequent IV medications, feeding tubes, or advanced wound care are in the picture, skilled nursing’s clinical depth becomes the deciding factor.
Costs vary widely by region and services. As a directional sense, monthly fees for assisted living often land in the mid‑to‑upper thousands, while skilled nursing can reach five figures when room, board, and clinical care are included. Look beyond the headline price: ask how levels of care are billed, whether rate increases are capped, and what happens if needs change unexpectedly. A transparent contract and a clear staffing plan signal a well‑run operation.
When touring, use your senses and your notebook:
– Observe interactions: Are staff greeting residents by name?
– Taste a meal: Is it appealing, varied, and flexible for special diets?
– Review activity calendars: Do offerings match interests, not just fill space?
– Ask about staffing: Training, turnover, and coverage at night.
– Request recent inspection summaries and how issues were fixed.
Beyond amenities, pay attention to mood. A place that feels alive at 3 p.m. on a Tuesday often reflects a culture that supports both safety and joy.
Paying for Care: Budgeting, Benefits, and Smart Trade‑Offs
Money choices shape care choices, so build a clear budget early. Tally predictable income sources and typical expenses; then layer in care scenarios. In‑home personal care billed hourly can add up; a few hours daily may be manageable, while 24/7 coverage becomes expensive quickly. Adult day programs are usually priced per day or half‑day. Residential settings charge monthly base rates, with additional fees for higher levels of assistance. Skilled services ordered by clinicians may be subsidized or time‑limited depending on local policies, but ongoing custodial care is often paid out of pocket.
Funding help varies by country and region. Some public insurance plans cover medical, short‑term rehabilitation, or hospice care but not long‑term personal care. Means‑tested programs can assist with home help or residential costs for those who qualify. Employer benefits sometimes include caregiver support, counseling, or backup care resources. Long‑term care insurance, where available, can defray costs for home aides or residential care, though benefits depend on the policy’s terms and eligibility triggers.
Stretch resources by matching services to the highest‑impact needs. If mornings are toughest, schedule help then and supplement with meal prep or technology later. Consider the trade‑offs:
– Home with part‑time help: lower cost, stronger continuity, more family coordination.
– Adult day plus home help: social engagement, respite for caregivers, structured days.
– Assisted living: predictable support and meals, private space, variable add‑on fees.
– Skilled nursing: clinical intensity, comprehensive support, higher monthly expense.
Read contracts carefully. Watch for community fees, assessment charges, separate medication management fees, and how rate increases are handled. Keep receipts for potential tax deductions tied to medical or personal care, subject to local rules. A brief meeting with a qualified financial or legal advisor can prevent costly missteps and align resources with values.
Bringing It Together: Communication, Safety, and a Practical Roadmap
Care works best when it fits the person’s life story. Begin with a family huddle that centers the older adult’s voice. Capture preferences: daily routines, food likes, favorite music, faith or cultural practices, and non‑negotiables. Translate these into care instructions so helpers can follow suit. Use plain language and one page per topic; complexity hides in thick binders nobody reads.
Build a 90‑day plan with checkpoints. Choose one priority per month—reduce falls, improve nutrition, or increase social outings—and assign simple tasks. Maybe the first month focuses on a home safety sweep and new lighting; the second, on medication routines and a pill reminder; the third, on joining a local art group or walking club. Schedule brief reviews to decide what stays, what changes, and what can be simplified. Small improvements compound.
Prepare for the unexpected. Create an “in case” folder with identification, medication list, allergies, key contacts, and copies of care preferences such as treatment goals or decision‑makers for health and finances. Place a copy on the fridge for first responders and share digital versions with trusted people. For peace of mind, map who to call if a caregiver is sick or transportation falls through.
Caregivers need care too. Without breaks, even the most devoted helpers burn out. Rotate responsibilities, accept offers of help, and schedule respite the way you would a medical appointment. Signs it’s time to adjust the plan include: rising falls or near‑misses, unintentional weight loss, mounting caregiver fatigue, or long stretches of isolation. When one of these shows up, treat it as a helpful signal to revisit options.
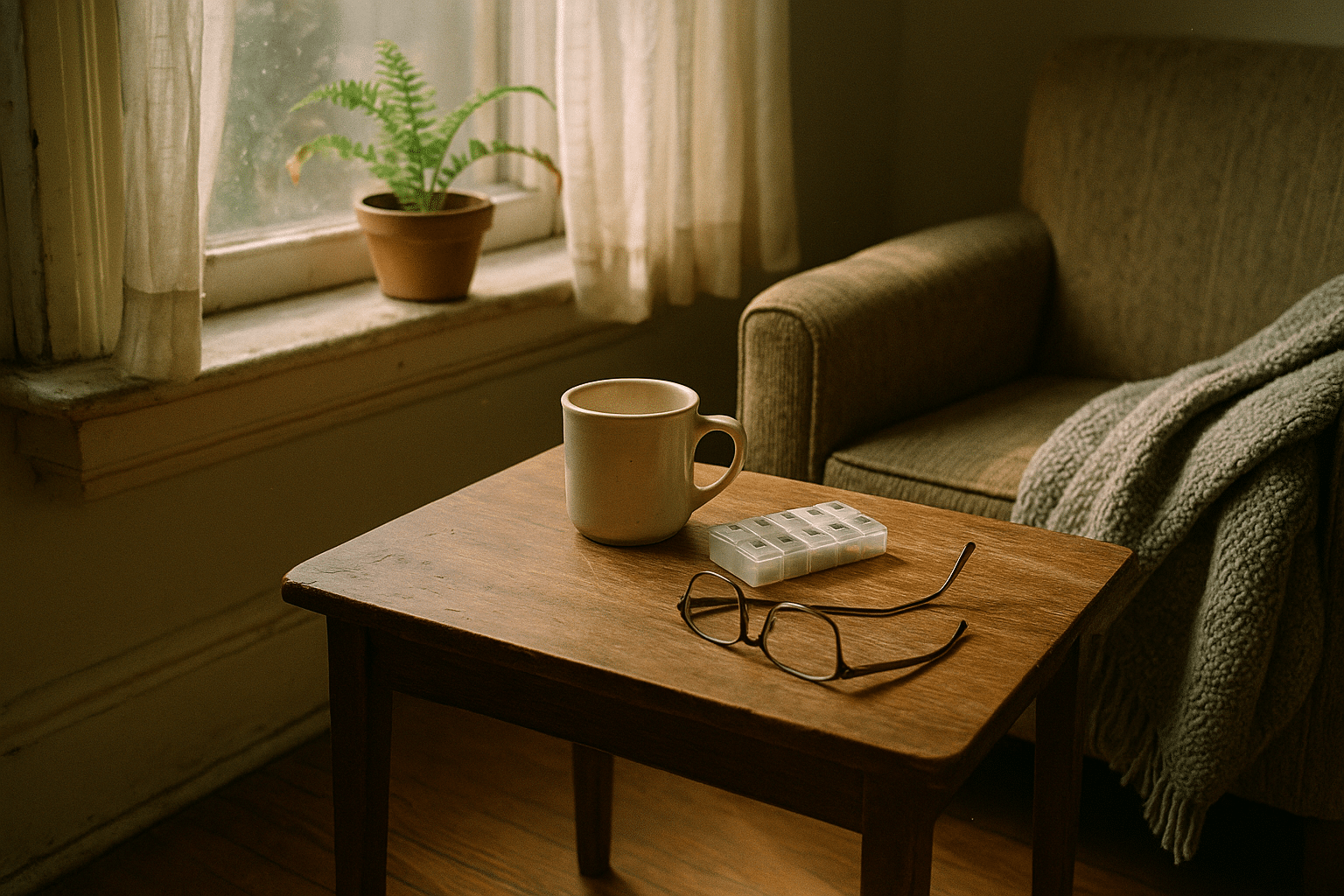
Conclusion for families: You don’t have to solve everything at once. Start with the clearest need, choose one support that meets it, and measure the difference. Add or pivot as life changes. With a grounded assessment, transparent costs, and honest conversations, you can assemble a care plan that protects safety, honors identity, and leaves room for ordinary joys—a favorite mug, sunlight on the kitchen table, and the comfort of a day well lived.